Michael's story
“The Select Specialty Hospital team was amazing.”
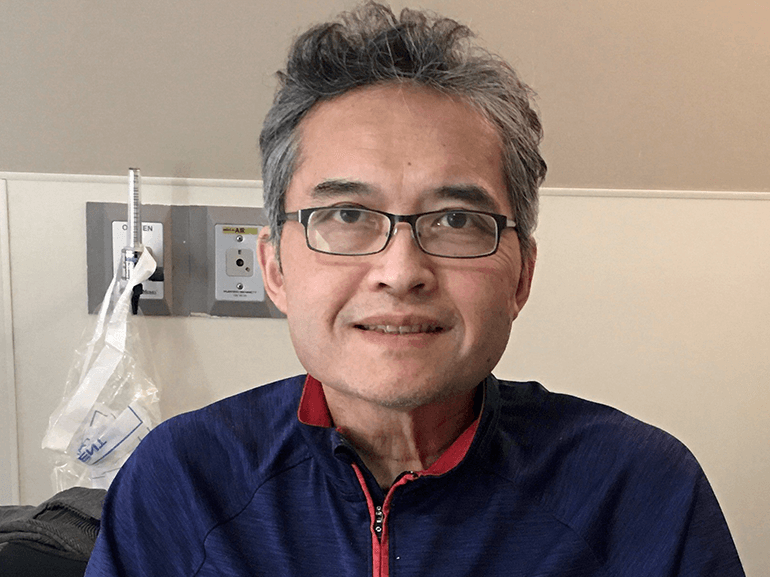
A physician heals from COVID-19
Dr. Michael Dao took every precaution to prevent contracting COVID-19. As a board-certified addiction medicine physician, caring for patients recovering from substance abuse was an essential part of combating the pandemic’s spread.
In July, however, Michael and his wife, Nathalie, came down with virus symptoms, including shortness of breath, fever and cough.
By month’s end, Michael’s condition deteriorated and he went to the local hospital’s emergency room. There, he fell into respiratory failure, was placed on a ventilator and underwent multiple treatments, including Dexamethasone, Remdesivir and convalescent plasma. By August, he’d been transferred to the intensive care unit at Vanderbilt Medical Center.
Between the disease and long hospital stay, Michael suffered delirium. Several sedating medications were administered to keep him from inadvertently pulling out tubes and lines. After 21 days, surgeons placed a tracheostomy and feeding tube.
In early September, Michael began to turn a corner and was transferred to Select Specialty Hospital – Nashville for extended recovery.
A physician-led team, including nurses and therapists, created a plan to help Michael get back on his feet and return to his family and practice.
To ease confusion, nurses and therapists routinely relayed the date, time, weather and tasks performed in the room. Pharmacists dialed back sedating drugs and optimized medication to ensure alertness during activity periods.
Physical and occupational therapists began Michael on a mobility program. First, they moved his arms and legs in range of motion exercises and encouraged in-bed movement. Each day, Michael improved, progressing to sitting, standing and walking with a walker.
Respiratory therapists stepped in to coach breathing and chest exercises, increasing lung function and stamina.
The delirium continued to present a significant challenge to recovery. After consulting with doctors and the medical director, Nathalie was cleared to stay in the hospital overnight with Michael in hopes of jolting his consciousness.
Michael recalled what it felt like to come back to himself. He believed he was still married to his first wife, and the nurses were trying to steal his identity. A practicing Buddhist, Michael comforted himself with three chants. By the end of the third, Nathalie walked into the room. He recognized her and his “clouded mind” cleared.
“My wife saved my life,” he said. “She constantly asked me where I was, showed me pictures of our daughters and family. She reminded me of our vacations and places we’d travelled.”
With increased awareness and improved oxygen levels, Michael was able to participate actively in physical and occupational therapy.
Speech therapists added a variety of cognitive and verbal activities to reconnect problem-solving, memory and planning abilities. They also used mouth, tongue and jaw exercises to retrain his swallowing reflex. Once tests indicated Michael could eat safely, dietitians crafted a meal plan that started with pureed and soft foods to ease his transition back to regular meals.
In October, three months after falling ill, Michael departed for an inpatient rehabilitation hospital to continue rebuilding his strength.
Several weeks later, some team members visited Michael at the rehab facility, and grabbed a photo of him using chopsticks to eat.
“The Select Specialty Hospital team was amazing,” he said. “The nurses were incredible. Even the ones who weren’t taking care of me stopped into say ‘hi’ and offer encouraging words about how far I’d come.”
Michael believes letting his diabetes get out of control contributed to his severe case. His advice? Get blood sugar and pressure under control. Eat well and lose weight if necessary.
Five and a half months later, Michael reports he is 90% recovered.
“I was able to get off the oxygen within two weeks of discharge,” he said. “The only lingering symptom is joint stiffness in the shoulders and fingers due to prolonged immobilization. We’ve worked up to a three-mile walk daily, I stretch regularly and eat a healthy diet. I still weigh 15 pounds less than I did before my hospitalization and plan to keep this weight permanently. I have returned to clinical practice, working about two to three days per week. We plan to travel to visit our friends and family as soon as the restrictions are removed.”