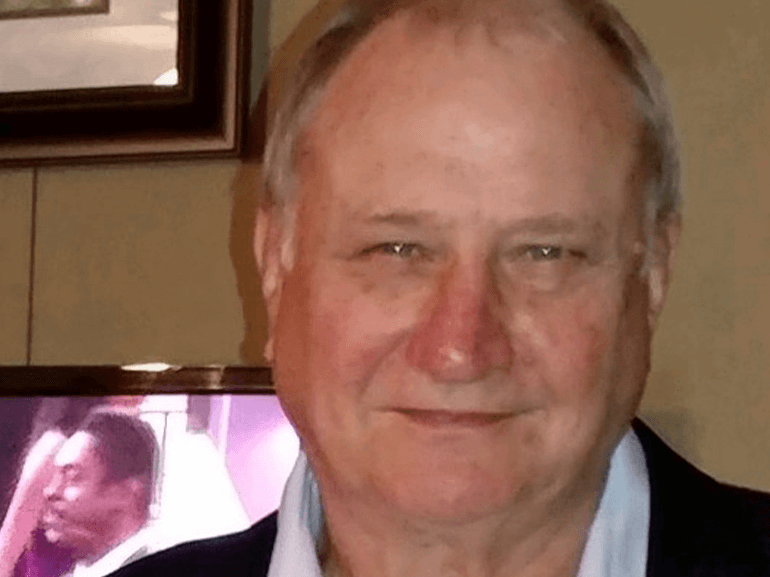
Robert's Story
Recovery after a routine procedure goes awry
It was supposed to be a routine outpatient procedure. At 71, Robert Culpepper went in for a colonoscopy, the common screening procedure for colon cancer. During the exam, doctors spotted and removed polyps to keep the growths from becoming malignant.
Twenty-four hours later, Robert was taken to the emergency room with nausea, vomiting and pain in his left side and abdomen.
Scans revealed a suspected perforation. One option was to wait and see if it healed on its own but that wasn’t going to work for Robert. He required surgery to repair the hole, remove abdominal abscesses and scar tissue.
Complications compounded as Robert needed several additional surgeries to remove a portion of his colon, install an ostomy, hernia repair and hematoma (blood-filled bruise).
Robert had been placed on a ventilator for the surgeries but was unable to liberate from the machine afterward. He endured a bloodstream infection, renal failure requiring dialysis and pneumonia. Eventually, a tracheostomy for airway support and feeding tube were connected.
After two months of intensive critical care, he stabilized enough for his adult son to consider the next step in healing. The family chose Select Specialty Hospital – Memphis because it is one of only a handful of facilities that accept patients on dialysis and a ventilator.
Robert arrived unable to breathe, eat, move, speak or think clearly. A previous stroke complicated his cognitive and verbal abilities.
The family’s goal was to get Robert off the ventilator and back to as much of his normal life as possible.
A physician-led team created a plan for success.
Respiratory therapy focused on twice daily, spontaneous breathing trials – short spurts of time with little or no ventilator support. This strengthened his lungs and gradually allowed Robert to be freed from the machine. He stepped down to a tracheostomy collar and special valve that permitted more normal speech.
Physical therapists began a mobility program to improve muscle strength and physical function. He started with bed exercises, rolling from side-to-side, moving toward the bed’s edge, sitting up and eventually moving to a chair. As Robert’s tolerance and endurance improved, therapists assisted in getting him to stand and turn with assistance.
Occupational therapists worked to rebuild dexterity in his upper extremities and overall cognitive function through puzzles, memory games, sorting activities and verbal commands.
Speech was one of Robert’s biggest hurdles. Exercises, activities, and repetition of sound improved his abilities to the point he could hold brief phone conversations with his wife. However, longer conversations continued to require much effort.
No matter how short, the phone and video calls were a lifeline to Robert, as visitation remained restricted due to COVID-19.
After a month and a half, Robert had made great progress. Several days before he was scheduled to leave for inpatient rehabilitation, his airway support was removed.
A week later, staff called to check up on him. His voice was clearer, stronger, and easier to understand. Robert was also improving physically and was hoping to walk independently soon.
He wanted to make sure the Select Specialty Hospital staff knew how grateful he was for their compassionate care.
“Everyone was so professional,” he said. “They were great.”