Julie's Story
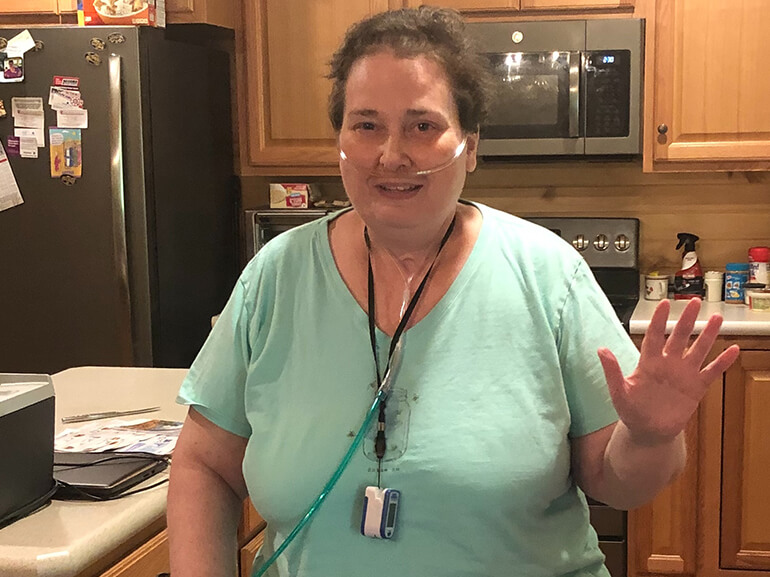
Julie Sherk, 51, works as a family nurse practitioner at UPMC. She is very involved with her church, teaches Sunday school and enjoys cross-stitching and tending to her wildflower gardens.
When she awoke feeling unwell, Julie took the day off and got a COVID-19 test. It was positive. Less than a week later, she was feeling worse and went to the local emergency department. An antibody transfusion was scheduled, but Julie’s oxygen levels dropped and she was admitted to UPMC Harrisburg.
Julie spent nearly two months in the hospital recovering from the virus, including time in the ICU and required mechanical ventilation. She experienced a deep tissue injury requiring wound care, a urinary tract infection, septic shock necessitating IV antibiotics and multiple blood transfusions. A tracheostomy for airway support and feeding tube were placed.
Once medically stable, Julie transferred to Select Specialty Hospital – Harrisburg. She arrived unable to breathe, eat or speak independently. Her skin injury required a pressurized dressing that needed close monitoring.
Julie’s main goal was to get off the ventilator so her physician-led team, including nurses and therapists, created a plan to help her get there.
Respiratory therapists and pulmonary critical physicians immediately started to work on getting Julie liberated from the machine. She credits one pulmonary critical care physician assistant for coaching her through every step of liberation. “I give her full credit for getting me off the ventilator,” Julie said.
Nurses tended her wound and monitored for signs of new ones. Eventually, the injury improved and the pressurized dressing was discontinued.
As a result of her medical issues, Julie developed nerve damage in her feet, was severely weak, unable to feed herself or turn over in bed. She also struggled with swallowing and speech as a result of being on the ventilator. Physical, occupational and speech therapists collaborated to restore eating, speaking and bed mobility skills with exercises that targeted key muscle groups.
Once off the ventilator, Julie’s next goal was to build endurance, begin walking and regain independence in daily living activities. After three months at Select Specialty Hospital – Harrisburg, she transferred to Helen M. Simpson Rehabilitation Hospital to continue recovery.
She arrived with airway support and feeding tube, needing five liters of oxygen while at rest.
Julie had made great progress, but much work remained. She struggled with personal care routines, needed two people to move her in bed and three to transfer between surfaces. Her oxygen needs increased with the slightest exertion.
Her physician-led rehabilitation team created a plan focused on increasing Julie’s strength, mobility and independence.
A week and a half after arriving at Helen M. Simpson Rehabilitation Hospital, Julie discontinued both the feeding tube and trach.
Physical therapists helped her become more adept at using a lift device and transfer board to move between surfaces. Julie said it was a major milestone when she could pull herself up in the lift. It meant to she was truly on the road to recovery.
As her legs grew strong enough to stand and manage taking steps, physical therapists placed her between the parallel bars, starting with just two to four at a time. Over time, she began taking more steps and could propel her wheelchair 50 feet.
Occupational therapists led activities geared to increase Julie’s ability to care for herself, such as brushing her teeth and getting dressed. Therapy also focused on family training and ordering proper adaptive equipment to ensure a safe discharge home.
“The therapists were great, going above and beyond to find equipment that would work for me,” Julie said. “I feel like I became friends with everyone.”
She also expressed her gratitude for the support her parents and church family showed throughout her hospital stay. Julie’s mother visited every day, took care of her finances, paperwork and the insurance coverage. The children in her Sunday school class sent pictures and cards to boost Julie’s spirits while their parents and other members took turns mowing her grass or providing financial assistance.
After 22 days, Julie departed for her parents’ house, where she was assisted with home therapy and nursing. Though her recovery journey wasn’t over, she was able to complete daily living activities and get around with greater independence. Julie couldn’t wait to see her friends and spend time with family.
She gives this advice to other patients in a similar situation: “Listen to the staff and focus on how far you have come and not how far you have to go.”